November 13, 2025
By Adjoa Kyerematen
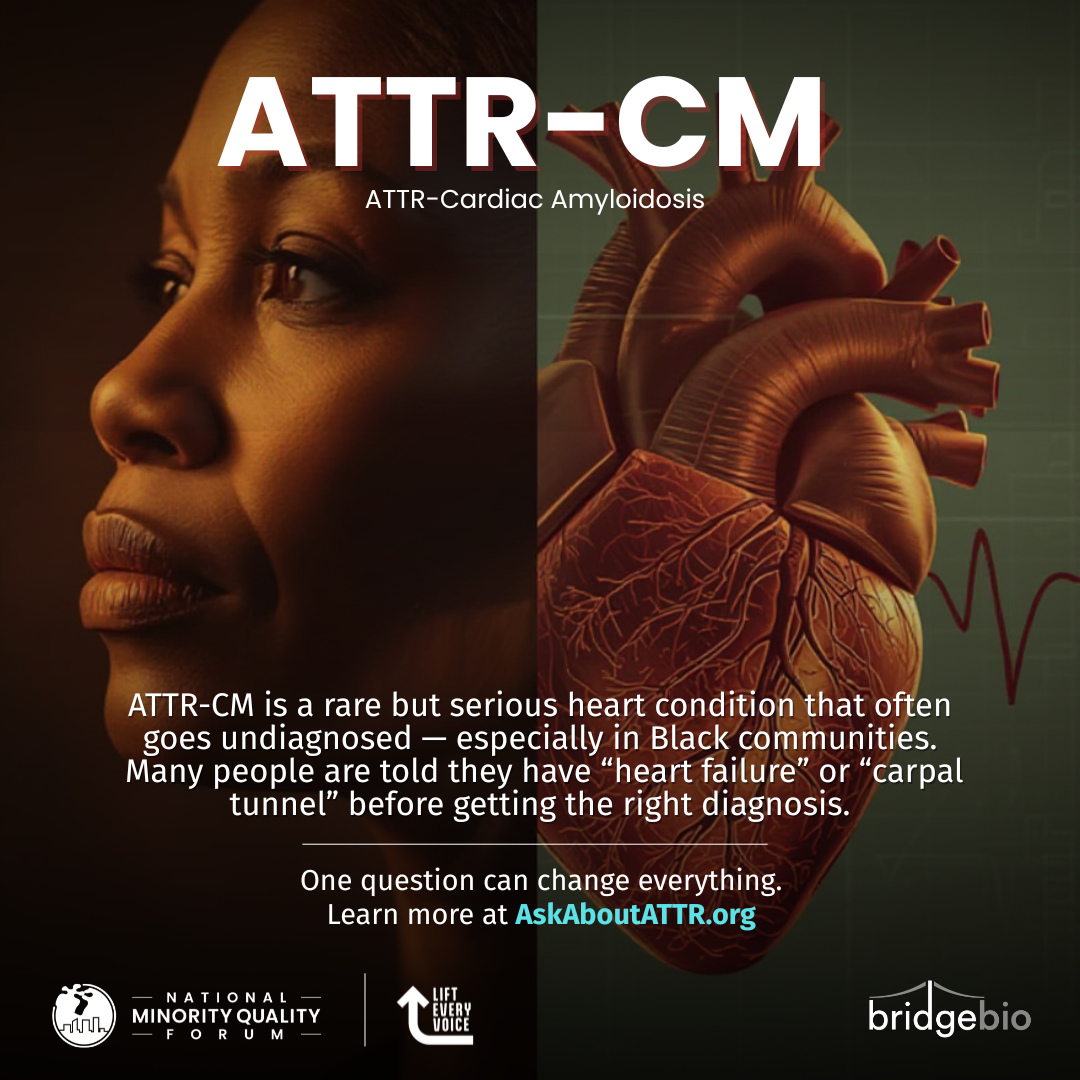
National Minority Quality Forum Launches AskAboutATTR.org to Empower Communities with Knowledge on Rare Heart Condition
Read More

9 July 2018
Sponsored By:
The New Democrat Coalition
The Congressional Black Caucus Health and Wellness Task Force
The National Minority Quality Forum (The Forum) is a not-for-profit, non-partisan organization that produces evidence-based research and analyses based upon zip code level health and socio-economic data. The Forum places a priority on the promotion of the innovation and investment that are essential to the creation of a healthcare research, financing, and delivery system that is inclusive of all populations, and that assigns equal priority to assuring the quality of healthcare that is available for and provided to all populations.
The Forum is concerned that current efforts to increase the scope and funding for Comparative Effectiveness Research are building a healthcare future upon an imperfect present. These imperfections include well-documented gaps in clinical evidence,[i] and the flawed premise that there is a single population “norm” against which healthcare quality standards can be established, thus eliminating what are reputed to be inappropriate practice and regional cost variations.
Unfortunately, most comparative effectiveness studies that have been released to date have offered sweeping generalities that largely ignore patient variability. The exclusion of women, minorities, children, and the elderly from clinical trials has resulted in a body of evidence that is inadequate to support conclusions that are generalizable to the population as a whole. In 2002, the editors of the New England Journal of Medicine observed, “Minority groups are underrepresented in most clinical trials. Often, there are insufficient data to assess the effectiveness or safety of new drugs in members of minority groups, especially blacks.” Their assessment remains true today. The Forum’s concerns are reinforced by reports issued by the NHS R&D Health Technology Assessment Programme[ii] for the UK’s National Health Service, and the Baylor College of Medicine Eliminating Disparities in Clinical Trials (EDICT) Project[iii].
The HTA report, The causes and effects of socio-demographic exclusions from clinical trials notes that, “In general, the exclusion from trials of those who are seen as ‘different’ or would require increased resources to be included…cannot be defended ethically and is against the principle of wide inclusion criteria to maximize generalizability of trial findings.”[iv] The HTA report also notes, “Under-representation occurs, but in drug trials at least this may not always affect the external validity of relative effect estimates. However, measures of absolute effectiveness, absolute harm and cost-effectiveness are associated with underlying risk levels in different socio-demographic groups. Under-representation will therefore bias absolute effect estimates.”[v]
Major Deficiencies in the Design and Funding of Clinical Trials, issued by EDICT in April 2008, reported that, “When it comes to the makeup of clinical trials, the National Institutes of Health requires that women and members of minority groups be included in all NIH-supported biomedical and behavioral research projects involving human subjects. Despite this requirement, little measurable improvement has been made in increasing clinical trials participation in such populations.”[vi]
Most importantly, the EDICT report states that, “Under-representation of specific populations in clinical trials is also at direct odds with the current state of medical science and drug discovery. With the successful sequencing of the human genome, scientists are faced with the new challenge of documenting, describing, and understanding the non-random pattern of human genetic variation and its link to disease risk in different patient groups. Findings from the large amount of genetic data generated to date show that more than 90 percent of the observed genetic variations occur within rather than between groups. This underscores the fact that ethnicity — which incorporates multiple variables including genetics, economic, social, dietary, religious, and linguistic background — has biomedical consequences when studying health outcomes.”[vii]
The Forum submits that any attempt to establish care norms or standards must take into consideration the following facts:
A long-standing lack of racial, ethnic, age and gender inclusiveness in randomized clinical trial cohorts;
The well-documented changing population demographics. It is projected that by the year 2020, approximately 40% of the American population will be composed, collectively, of population groups that are currently defined as racial/ethnic minority populations, increasing to 50% of the American population by 2050;[viii]
Well-documented biases in the manner in which health care is delivered to different racial/ethnic groups (see IOM “Unequal Treatment”);
Well-documented disparities in access to treatment resulting from uninsurance and under-insurance for different racial/ethnic groups; and
Ongoing research into genomic and biological markers for disease as well as differential responses to pharmacological agents.
As Congress endeavors to reform the health care delivery and financing system fulfill this specific charge from Congress, the National Minority Quality Forum encourages you to consider the following questions:
Can Comparative Effectiveness Research be conducted and applied in a scientifically-based and clinically valid manner for all racial, ethnic, age and gender population cohorts?
Do the necessary data sources, analytical constructs, and methodological tools currently exist to conduct comparative effectiveness research and produce relevant and scientifically-based findings for the diverse ethnic, racial, gender, and age cohorts that are America?
Is the American healthcare research, delivery and financing system designed to provide high quality, cost-effective care to all in an equitable manner?
Do the operational structures for current and proposed national comparative effectiveness research initiative include formal structures and/or processes to ensure broad public input and transparent decision-making as priorities are determined and research is undertaken.
Do the proposed priorities for comparative effectiveness research include populations for whom a lack of scientific data currently exists, including research on at-risk and underserved populations, individuals with disabilities, and the chronically ill.
Does the approach to CER that is being designed or implemented focus on the development of appropriate clinical evidence?
Are guidelines and/or standards regarding levels of evidence being applied consistently across populations, conditions, treatments, and devices
The National Minority Quality Forum is concerned that until the answer to each of these questions is “Yes”, that Comparative Effectiveness Research may serve to establish different standards of quality that continue an unfortunate history of bias and lack of inclusion within the healthcare research, delivery and financing system. From a pragmatic perspective, however, if Comparative Effectiveness Research is to be undertaken in an environment in which the answer to each of the aforementioned questions is not yet “Yes”, then The Forum strongly encourages Congress to strengthen the protections for all Americans by assuring that healthcare reform proposals contain the following provisions:
Ensure that any current or newly created CER entities be established as public-private partnerships with representation and joint decision-making from all stakeholders, and be ruled by consensus. This will help to ensure that decisions are reached objectively and are not dominated by any one set of stakeholder interests.
Require that CER studies that are supported in whole or in part by federal funds report on emerging populations, unless an explicit wavier is granted. The granting of a waiver must adhere to strict guidelines established in the legislation.
Require that CER studies that identify a gap in evidence for an emerging population immediately make closing that gap a priority.
·Require that all CER reports contain a clear statement that defines the patient cohorts for whom the research findings are valid and applicable.
Require that all purchasers and/or payers who base coverage decisions, in part or in whole, on CER findings collect data and report beneficial and adverse changes in outcomes for the beneficiaries who are subject to those coverage decisions in a manner that clearly identifies the effect by age, gender, racial/ethnic, geographic and economic cohorts.
Require the CER entity to provide support for the dissemination of study findings in a manner that is linguistically and culturally competent.
Appropriate funds to build and sustain CER institutes within Morehouse College and the Charles Drew School of Medicine as part of the commitment to increase diversity within the research community.
As stated in the requirement for implementation outlined in Section 1013 (b)(2) of H.R.1, Medicare Prescription Drug, Improvement, and Modernization Act of 2003:
Research, evaluation, and communication activities performed pursuant to this section shall reflect the principle that clinicians and patients should have the best available evidence upon which to make choices in health care items and services, in providers, and in health care delivery systems, recognizing that patient subpopulations and patient and physician preferences may vary.
The National Minority Quality Forum believes these recommendations will strengthen the ability of Congress and all relevant departments within the Executive and Judicial Branches of the Federal Government to comply with this directive, and will help assure that citizens receive quality healthcare that is defined by the independent judgment of the provider based upon the needs of individual patients.
In closing, knowing and understanding the diversity of the patients in the healthcare system will enable the healthcare system to stimulate investment in healthcare quality in a manner that both improves cost-effectiveness, and builds a more efficient system that is powered to sustain a more diverse American in the 21st century… and beyond. The National Minority Quality Forum looks forward to working with Congress on these critical issues.
Footnotes
[i] Obtained either through randomized clinical trials or observational studies.
[ii] One of the programs that informs the NICE decision-making process is the NHS R&D Health Technology Assessment Programme.
[iii] EDICT is a research partnership between the Intercultural Cancer Council and the Baylor College of Medicine in Houston that aims to improve the participation of minorities and undeserved patients in clinical research trails.
[iv] Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al. The causes and effects of socio-demographic exclusions from clinical trials. Health Technol Assess 2005; 9(38), page 100.
[v] Ibid, page iv.
[vi] Chronic Disease Prevention and Control Research Center at Baylor College of Medicine, in collaboration with the Intercultural Cancer Council. Major Deficiencies in the Design and Funding of Clinical Trials: A Report to the Nation Improving on How Human Studies Are Conducted. Findings of the Eliminating Disparities in Clinical Trials Project (EDICT), April 1, 2008, page 8.
[vii] Ibid, page 9.
[viii] The demographics of the US population are shifting away from a single racial/ethnic group majority. According to the US Census Bureau’s 2005 mid-decade estimates, approximately 1-in-every-3 U.S. residents is part of a group other than single-race non-Hispanic White. In 2005, the nation’s minority populations totaled 98 million, or 33 percent, of the country’s total of 296.4 million. It is projected that by the year 2020, approximately 40% of the American population will be composed, collectively, of these racial/ethnic minority population groups, increasing to 50% of the American population by 2050. Given the relatively younger ages of the minority population groups, it can be assumed that an increasing percentage of the American work force and school age children will be members of population groups that are currently classified as non-Hispanic single race Caucasian.
About The Forum
The National Minority Quality Forum (NMQF) is a 501(c)(3) not-for-profit, non-partisan, independent research and education organization. The vision of NMQF is a health services research, delivery and financing system that provides quality and effective health services to the biodiverse American general population of the 21st century. NMQF helps assure that national and local quality improvement initiatives are informed by scientific evidence, and place a priority on the quality of care and patient outcomes in all populations.